02 Oct 23
Using AI and ML to Revolutionise Early Breast Cancer Detection
In recent years, the integration of artificial intelligence (AI) and machine learning (ML) into the realm of medical science has been nothing short of revolutionary. One of the most promising applications of this technology is in the early detection of cancer. By leveraging the power of AI and ML algorithms, researchers and medical professionals have made significant strides in improving the accuracy and efficiency of cancer detection, particularly in cases of breast cancer.
In this blog, we will delve into how AI is transforming the landscape of early breast cancer detection and diagnosis. Specifically, we’ll explore its successes, and shed light on some potential challenges that need to be addressed.
AI in Early Breast Cancer Detection
Breast cancer is one of the most prevalent forms of cancer in women and according to the World Health Organisation, more than 2.3 million women develop the disease every year. AI has shown remarkable potential in this domain.
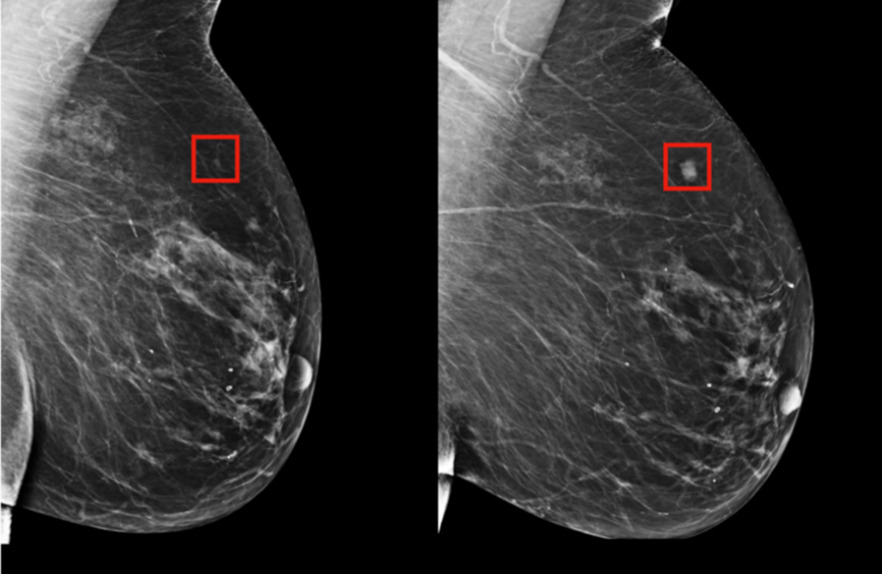
Machine learning algorithms are capable of analysing mammograms and identifying patterns that might be difficult to discern by the human eye. Through pattern recognition, AI systems can assist radiologists in detecting even the subtlest signs of abnormalities, potentially leading to earlier diagnosis and better patient outcomes.
In a groundbreaking collaboration between MIT’s CSAIL and Massachusetts General Hospital, an advanced deep learning model has emerged, capable of predicting breast cancer up to five years in advance. By analysing mammogram images and recognizing subtle precursors to tumours, this model, trained on a vast dataset of 90,000 mammograms, exhibits unprecedented accuracy. It identifies 31 percent of high-risk patients, compared to the 18 percent recognized by conventional methods. This innovation holds the potential to revolutionize early intervention and personalized treatment plans.
This milestone underscores the transformative role of AI in healthcare, offering a glimpse into a future where technology plays a pivotal role in predicting and preventing diseases. By foreseeing breast cancer risks five years ahead, medical professionals can take proactive measures, improving patient outcomes and lessening the impact of the disease.
How does AI mammography work?
Step 1: Data Collection and Preparation
A large dataset of mammograms, containing both normal and abnormal cases, is collected. These images serve as the training data for the AI algorithm.
Step 2: Feature Extraction
AI algorithms use feature extraction techniques to identify specific patterns, textures, and shapes in the mammogram images. These features might include edges, masses, microcalcifications, and other characteristics associated with breast cancer.
Step 3: Model Training
Using machine learning techniques such as convolutional neural networks (CNNs) or other deep learning architectures, the AI model is trained on the pre-processed mammogram dataset. The model learns to recognize patterns indicative of normal and abnormal cases.
Step 4: Learning Patterns
During training, the AI model learns to associate image features with specific classes (normal or abnormal, as well as subtle signs that might be hard to identify with the naked eye.
Step 5: Validation and Testing
The trained model is validated using separate datasets to ensure that it can generalize well to new, unseen cases. It’s crucial to validate the model’s accuracy and performance to avoid overfitting or biased results.
Step 6: Continual Learning
Some AI systems are designed for continual learning. As new data becomes available, the model can be updated to improve its performance over time. This is particularly important for adapting to new cases and variations in breast cancer presentations.
Challenges and Caution
While early breast cancer detection using AI and mammograms offers promising advantages, there are also several challenges and risks that need to be carefully considered:
False Positives and False Negatives: AI algorithms can sometimes produce false positives (indicating cancer where there is none) or false negatives (missing actual cases of cancer). Balancing sensitivity and specificity is crucial to avoid unnecessary anxiety for patients due to false alarms or missed diagnoses.
Over-Reliance on Technology: Relying solely on AI for interpretation could lead to a reduced emphasis on the expertise of human radiologists. Human oversight and judgment remain essential to validate AI-generated results.
Ethical and Legal Concerns: Ensuring patient privacy, data security, and compliance with regulations like HIPAA is paramount.
Validation and Generalization: AI models need to be validated on different datasets and populations to ensure they generalize well to new cases. What works well on one dataset might not perform similarly on another.
Patient Anxiety and Psychological Impact: False positives and the mere mention of AI in medical diagnosis can lead to heightened anxiety among patients. Proper communication and support mechanisms are crucial to address psychological impacts.
Continuous Research is Needed
AI and machine learning are revolutionising early cancer detection by harnessing the power of data analysis, pattern recognition, and speed. With the ability to analyse medical images and patient data swiftly, these technologies have the potential to save lives by enabling earlier diagnosis and intervention.
However, striking a balance between the undeniable benefits of AI and the potential risk of overreliance is essential. As AI continues to evolve, ongoing research, collaboration between medical professionals and technologists, and continuous improvement will be vital in realizing the full potential of AI in the fight against cancer.
Interested in joining our diverse team? Find out more about the Rockborne graduate programme here.
Related posts
Life at Rockborne20 Jun 25
Federated Learning: The Future of Collaborative AI in Action
Federated Learning: The Future of Collaborative AI in Action The way we build, deploy, and govern AI is evolving, and so are the expectations placed on organisations to do this...
09 Sep 24
Tips to Succeed in Data Without a STEM Degree
By Farah Hussain I graduated in Politics with French, ventured into retail management, dabbled in entrepreneurship, a mini course in SQL and now… I am a Data Consultant at Rockborne....
15 Apr 24
Game Development at Rockborne: How is Python Used?
Just how is Python used in game development? In this blog post, we see the Rockborne consultants put their theory into practice. As the final project in their Python Basics...

